Abstract
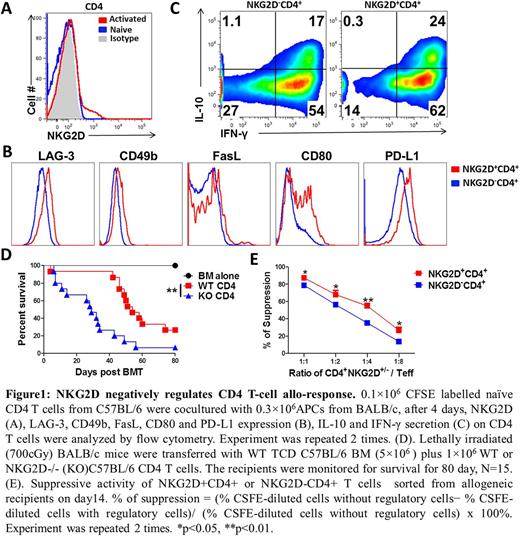
NKG2D is a C-type lectin-like receptor which mainly expresses on mouse NK, activated CD8 and some γδ T cells. NKG2D is also found to express on human and mouse CD4 T cells, but the role of NKG2D in CD4 T cells is essentially unknown. We asked what subsets of CD4 T cells could express NKG2D; we activated and polarized CD4 T cells into Th0, Th1,Th2, Th17 and Foxp3+ Tregs in vitro and measured NKG2D expression on those subsets. We found that only a proportion of Th1 cells expressed NKG2D, whereas little or no NKG2D was expressed on other subsets of T cells. In a mixed lymphocyte reaction (MLR) assay, NKG2D was induced on a subset of CD4 T cells after stimulation with allogeneic antigen presenting cells (APCs) (Figure 1A). NKG2D+CD4+ T cells expressed higher levels of LAG-3, CD49b, CD80, FasL and PD-L1 (Figure 1B) and secreted more IL-10 and IFN-γ than NKG2D- CD4+ T cells (Figure 1C).
Previous reports by others showed that NKG2D on NK and activated CD8 T cells contributing to graft versus host disease (GVHD) pathogenesis have been well-established, but the expression and function of NKG2D on CD4 T cells in GVHD development are unknown.
To address these questions, we utilized a CD4-driven, MHC-mismatched aGVHD model of allogeneic bone marrow transplantation (allo-BMT), C57BL/6 to BALB/c. We monitored the development of NKG2D+CD4+ T cells in allogeneic recipients. We observed that NKG2D was continuously induced on CD4 T cells during the whole aGVHD process - gradually increased, peaked on day 14 and then slowly decreased after allo-BMT. By comparing the severity of aGVHD in recipients transferred with WT versus NKG2D-/- CD4 T cells. We observed that recipients transferred with NKG2D-/- CD4 T cells showed more severe GVHD demonstrated by a higher lethality (Figure 1D) and more severe diarrhea compared to WT counterpart. Mechanistically, NKG2D-/- CD4 T cells had a higher capacity of migrating to gut and liver than WT CD4 T cells reflected by the higher expression of α4β7 and CXCR3. Furthermore, NKG2D+CD4+ T cells secreted less proinflammatory cytokine IL-17 and more anti-inflammatory cytokine IL-10. Strikingly, NKG2D expression coincided with T-bet, but excluded RORγt or Foxp3 expression of CD4 T cells. Given NKG2D+CD4+ T cells expressed regulatory markers and secreted IL-10 and IFN-γ; we hypothesized that NKG2D+CD4+ T cells may serve as suppressive cells (e.g. Tr1 cells). To test this hypothesis, we sorted NKG2D+CD4+ and NKG2D-CD4+ T cells from recipients of allogeneic BMT, and performed in vitro suppressive assay. We observed that NKG2D+CD4+ T cells had a higher suppressive activity than NKG2D-CD4+ T cells. (Figure 1E)
Taken together, the current work demonstrates that NKG2D may serve as a negative regulator on CD4 T cells, and NKG2D+CD4+ subset can function as a regulatory cell subset in the development of GVHD after allo-BMT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal